Science
AI Algorithms Revolutionize Brain Metastases Treatment Efficiency
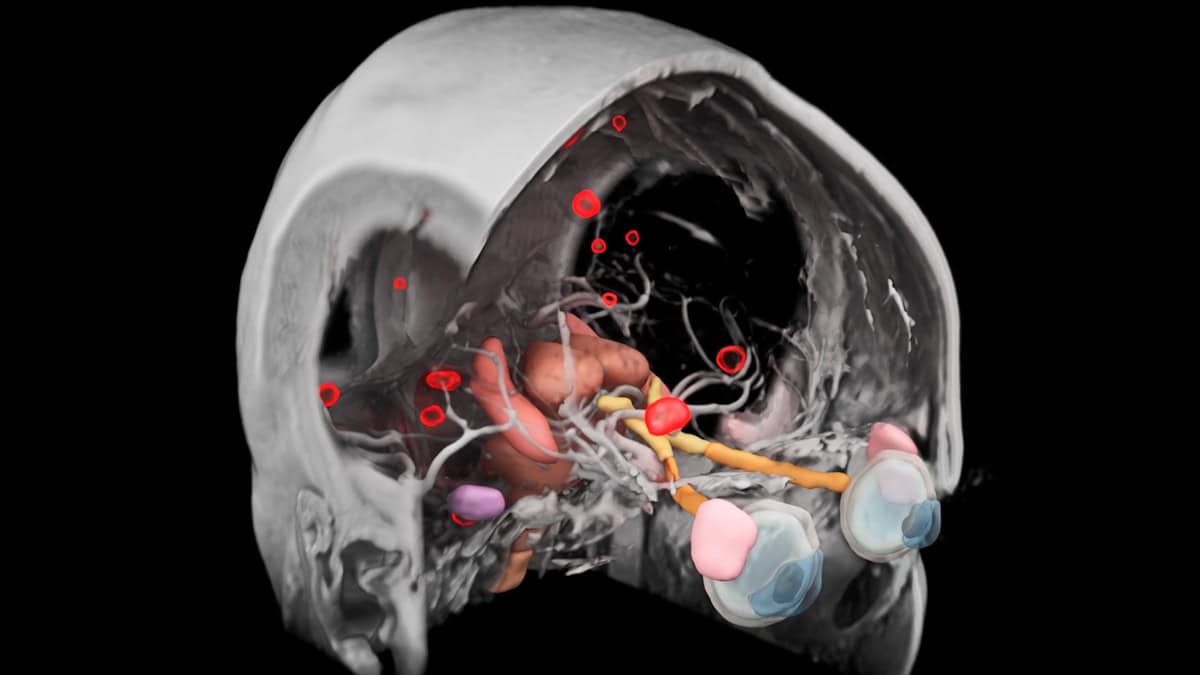
Recent advancements in artificial intelligence are transforming the treatment of brain metastases, cancerous lesions that spread from other body parts. A new software tool developed by Siemens Healthineers automates the contouring process for stereotactic radiotherapy (SRS), significantly enhancing accuracy and efficiency in identifying and treating multiple lesions.
Brain metastases are increasingly managed through SRS, which delivers high doses of radiation to individual lesions. This method is preferred over whole-brain irradiation due to its ability to provide better local control and cognitive preservation while shortening treatment duration. However, the initial step of detecting and delineating lesions on MRI scans can be complex and time-consuming. According to Evrim Tezcanli, a professor of radiation oncology at Acibadem Atasehir Hospital in Turkey, effective treatment requires careful identification of all lesions. “Very small lesions, particularly those under 0.1 cc, can easily be missed by untrained eyes,” she notes.
AI-Powered Contouring Tool Enhances Precision
To address these challenges, Siemens Healthineers’ new AI software, integrated into their syngo.via RT Image Suite and AI-Rad Companion Organs RT packages, employs advanced deep-learning algorithms. This software swiftly analyzes MRI images, automatically contouring and labeling metastatic lesions while identifying critical organs at risk, such as the brainstem and optic structures. “One of the main strengths of this software is that it reduces the manual workloads significantly,” Tezcanli adds.
A study conducted by Tezcanli and her team evaluated the new software’s accuracy against the performance of two experienced radiation oncologists. The research included data from ten patients with three to seventeen brain metastases. The oncologists manually contoured all 82 lesions based on the patients’ contrast-enhanced MRI scans, while the AI processed the same images for automatic contouring.
The results indicated impressive performance from the AI software. Tezcanli reported strong agreement between manual and AI-generated contours, particularly for lesions larger than 0.1 cc. The study revealed a medium Dice similarity coefficient of 0.83, which improved to 0.91 when omitting very small lesions. Additionally, the median Hausdorff distance, the maximum discrepancy between the two contour types, was recorded at 0.3 mm.
Time Savings and Clinical Implications
The time efficiency of the AI tool was another focal point of the study. The researchers compared the duration spent on contouring by the radiation oncologists with the automated process. The AI software completed contouring for each patient in just one to two minutes, resulting in an average workload reduction of 75%. In some cases, this automation saved over 30 minutes per patient. “We still needed to review the AI contours, but the correction time was only three to four minutes,” Tezcanli explains, underscoring the continued necessity for expert review.
From a patient perspective, the implications of AI-based contouring are significant. Reducing the time spent on manual contouring allows physicians to dedicate more time to patient interaction. This is especially vital in a field where timely treatment is crucial for patient outcomes.
The study utilized post-contrast T1 MPRAGE sequences recorded with a 3 Tesla MRI scanner to maximize lesion visibility. The sensitivity of the software was impressive, achieving an overall detection rate of 94%, successfully identifying 77 out of 82 metastases. While five lesions were missed, they were exceptionally small, between 0.01 to 0.03 cc. Notably, the AI tool also detected three additional lesions that had not been identified initially, later confirmed as metastases.
Some limitations were noted, including an 8.5% false positive rate, where the software mistakenly identified vascular structures as metastases. Tezcanli cautions that vascular enhancements can mimic tumors, necessitating careful examination with dedicated MRI sequences.
The contours generated by the AI software are exported in DICOM RT Struct format, facilitating direct transfer into treatment planning systems. At Acibadem Atasehir Hospital, this process is streamlined using HyperArc, a specialized software module for radiosurgery that automates treatment planning and delivery, making SRS both fast and efficient.
“HyperArc has proven to be highly effective, even when treating patients with multiple brain metastases,” remarks Burcin Ispir, a medical physicist collaborating with Tezcanli. The software’s ability to perform single isocentre, automated planning for multiple targets significantly reduces planning time while maintaining high treatment quality.
The integration of AI in contouring and HyperArc in planning accelerates the overall treatment process. This efficiency allows for potentially earlier commencement of radiation therapy, which is crucial for patients receiving concurrent systemic treatments. Tezcanli emphasizes the importance of timely intervention: “We are in an era where we are using the technology to have even same-day treatments.” With rapid AI contouring, quick expert reviews, and efficient planning, patients can often start their treatment within hours of their MRI scan.
Looking ahead, advancements in cancer treatment methodologies suggest a growing role for SRS in managing brain metastases. “I think we will be treating brain metastasis more and more,” Tezcanli asserts. She believes that SRS will become the primary treatment modality, with AI playing a key role due to the time savings and accuracy it offers. “This is only the first version of the software; I’m sure it can be improved to find even smaller lesions or differentiate vascular structures.”
While the software has not yet been fully integrated into routine practice, Tezcanli expresses confidence in its potential for future use. “I think we will be using it routinely in the future in all of our clinical cases,” she concludes.
The statements made by customers of Siemens Healthineers are based on unique results achieved in specific settings. As hospital environments vary significantly, outcomes may differ. The products mentioned are not universally available, and their future availability is not guaranteed.
-

 Entertainment2 months ago
Entertainment2 months agoIconic 90s TV Show House Hits Market for £1.1 Million
-

 Lifestyle4 months ago
Lifestyle4 months agoMilk Bank Urges Mothers to Donate for Premature Babies’ Health
-

 Sports3 months ago
Sports3 months agoAlessia Russo Signs Long-Term Deal with Arsenal Ahead of WSL Season
-

 Lifestyle4 months ago
Lifestyle4 months agoShoppers Flock to Discounted Neck Pillow on Amazon for Travel Comfort
-

 Politics4 months ago
Politics4 months agoMuseums Body Critiques EHRC Proposals on Gender Facilities
-

 Business4 months ago
Business4 months agoTrump Visits Europe: Business, Politics, or Leisure?
-

 Lifestyle4 months ago
Lifestyle4 months agoJapanese Teen Sorato Shimizu Breaks U18 100m Record in 10 Seconds
-

 Politics4 months ago
Politics4 months agoCouple Shares Inspiring Love Story Defying Height Stereotypes
-

 World4 months ago
World4 months agoAnglian Water Raises Concerns Over Proposed AI Data Centre
-

 Sports4 months ago
Sports4 months agoBournemouth Dominates Everton with 3-0 Victory in Premier League Summer Series
-

 World4 months ago
World4 months agoWreckage of Missing Russian Passenger Plane Discovered in Flames
-

 Lifestyle4 months ago
Lifestyle4 months agoShoppers Rave About Roman’s £42 Midi Dress, Calling It ‘Elegant’